There are many barriers to public benefits enrollment. Low income workers who qualify for these benefits often don’t have the time to take off work and spend hours navigating the complex system. In some cases, people can save significantly on healthcare costs by enrolling in Medicaid rather than their company plan, but going through the process can seem insurmountable without support.
BeneStream is a guide and advocate for people who often don’t know that they’re eligible for public benefits and are too busy to complete the process. They work with companies to register their employees for Medicaid and other types of benefits, navigating the arcane and bureaucratic process of health care enrollment to find the package that’s best for them.
BeneStream performs its work primarily through phone calls and in-person assistance. But when you’re dealing with thousands of people negotiating a complex system, there is inevitably a tremendous amount of follow-up.
BeneStream looked for a way to conveniently keep track of its customers after the phone calls had ended. Many of BeneStream’s employee clients don’t have smartphones, and find text messaging a more comfortable and convenient service.
BeneStream realized that a text messaging campaign could provide personalized follow-up to thousands of people at a minimal resource cost and in a convenient way to its employee clients.

How It Works
Tracking Enrollment
BeneStream schedules phone calls with their clients’ employees to walk them through health care enrollment. They’ll stage three-way calls with the customer and a state employee to make sure the person gets enrolled.
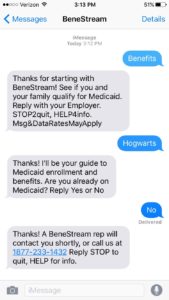
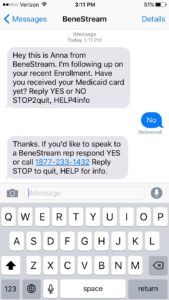
But with a system as complex as Medicaid, mistakes can still get made. BeneStream needs to make sure those Medicaid cards arrive just like they’re supposed to.
“We use Upland Mobile Messaging to follow up,” said Rebecca Karasik, BeneStream’s Director of Product. “We’ll send an automated text a few weeks after the call, asking people if they received their Medicaid card yet. If they say no, we follow up again a few weeks later.”
Tracking Eligibility
One of the challenges of Medicaid enrollment is that people may go in and out of eligibility. Many of BeneStream’s employee clients have variable work hours, and as a result their economic situation changes throughout the year. Using Upland Mobile Messaging, BeneStream is able to easily keep in touch and keep track of changing situations. “If we were to try to call people on the phone, they’d be too busy and wouldn’t pick up,” said Karasik “But they will respond to a text.”
BeneStream pings their non-enrolled customers every month to check in on their status. If they become eligible for Medicaid, then BeneStream can follow up with an enrollment phone call.
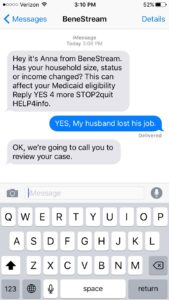
After this conversation, a BeneStream representative would follow up and enroll the user over the phone.
Tracking Required Documents
Another barrier to government benefits enrollment are the additional documents and follow-ups with government that individuals and their families need to send.
Sometimes, halfway through an enrollment, BeneStream will discover that the state requires more documents from a customer. Someone might need to prove their income, or verify the immigration status of their children. BeneStream will mark in their Customer Relationship Management CRM (software) that further documents are required. BeneStream will then send text message reminders to people to supply their information, and confirm that the correct information is sent to the state Medicaid office.
Reminding People to Renew
Unlike private insurance provided by an employer, the Medicaid renewal process can be unpredictable and takes time. BeneStream will text people annual reminders to renew their Medicaid starting 3 months in advance of the renewal date, and also offers more personalized help when required.
Personalized Support
BeneStream also uses text messaging to address more specific customer problems. Sometimes, people respond to BeneStream’s messages with more than a ‘Yes’ or ‘No’ answer. They might ask questions about eligibility or wonder where a missing Medicaid card is. Using Upland Mobile Messaging Agent View, BeneStream can offer personalized follow-up over text – or refer the issue to a phone agent.
“If we were to try to call people on the phone, they’d be too busy and wouldn’t pick up. But they will respond to a text.”
BeneStream also offers companies the option of creating specific keyword opt-in paths. “Sometimes, employees don’t understand how BeneStream is connected to their employer. But when they can text ‘Acme Corp Benefits’ and receive personalized help, they get the connection“ said Karasik.
BeneStream uses Upland Mobile Messaging’s segmentation and tracking tools to make sure they’re sending the right information to the right people. When BeneStream revamped its “30 Day Follow Up” campaign to ask for specific documents, their opt-out rate decreased from around 50% to 6%. “We’ve seen that when the text doesn’t read like a text blast, folks will respond,” said Karasik.
A System that Works for BeneStream & Its Employee Clients
Text message follow-ups and reminders are a simple way to keep in touch with a large amount of people, without the tremendous investment in resources that phone calls would require.
For BeneStream’s employee clients, many of whom often can’t afford a smartphone and work more than 40 hours a week, sending a text message is an easy way to keep track of their enrollment status, and if further support is required, BeneStream gets to know about it instantly.